Signs, Symptoms and Characteristics
Understanding Dup15q Syndrome
 Chromosome 15q11.2-13.1 duplication syndrome (Dup15q syndrome) is a clinically identifiable syndrome that results from the duplication (or multiplication) of a portion of chromosome 15.
Chromosome 15q11.2-13.1 duplication syndrome (Dup15q syndrome) is a clinically identifiable syndrome that results from the duplication (or multiplication) of a portion of chromosome 15.
Each chromosome has unique regions or bands that contain genes, and each band is labeled numerically. The extra genetic material known as Dup15q syndrome contains the bands on chromosome 15 at the q arm labeled 11.2-13.1.
It can span past these bands but must contain the 11.2 – 13.1 region to be identified as Dup15q syndrome. These duplications most commonly occur in one of two forms. These include an extra isodicentric 15 chromosome, abbreviated idic(15), or an interstitial duplication 15, abbreviated int dup(15).
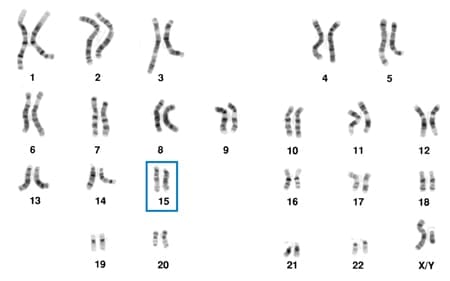 Chromosome 15 is one of the 23 pairs of chromosomes in humans. Humans are born with 2 copies of each chromosome – 1 from the mother (maternal) and 1 from the father (paternal). Depending on which parental chromosome the extra genetic material is on, symptoms may present differently. In most cases of chromosome 15q11.2-13.1 duplication syndrome, the chromosome duplication is not inherited, but de novo, which means the multiplication occurred as a random event during early embryonic development.
Chromosome 15 is one of the 23 pairs of chromosomes in humans. Humans are born with 2 copies of each chromosome – 1 from the mother (maternal) and 1 from the father (paternal). Depending on which parental chromosome the extra genetic material is on, symptoms may present differently. In most cases of chromosome 15q11.2-13.1 duplication syndrome, the chromosome duplication is not inherited, but de novo, which means the multiplication occurred as a random event during early embryonic development.
There are many other genetically derived names that are commonly used in the diagnosis for Dup15q syndrome, including; 15q11.2-q13.1 duplication syndrome, Inverted duplication 15 (inv dup15), Partial trisomy 15, Isodicentric chromosome 15 syndrome [Idic(15)], Supernumerary marker chromosome 15 (SMC15), Partial tetrasomy 15q, etc. All of these names describe the genetics of “Dup15q syndrome”.
Why does Dup15q syndrome fall under the definition of a “disease”? Disease is defined as a disorder of structure or function in a human that impairs normal functioning, manifested by distinguishing signs and symptoms.
Why is Dup15q called a “syndrome”? A syndrome is a term that refers to a disease or a disorder that has more than one identifying feature or symptom.
Dup15q syndrome is characterized by having an extra copy of a portion of chromosome 15 in the 11.2 – 13.1 region in combination with a number of symptoms that may include hypotonia and motor delays, intellectual disability, autism spectrum disorder (ASD), and epilepsy including infantile spasms. Rarely, maternal Dup15q may also be associated with psychosis or sudden unexplained death.
It is important to acknowledge that there is a wide range of developmental disabilities experienced by individuals with chromosome 15q11.2-13.1 duplication syndrome. Two individuals with the same Dup15q chromosome pattern may be very different in terms of their abilities. Reviews of the scientific literature do not show an obvious correlation between the size of the duplication region and the severity of the symptoms. However, the following features are found to some degree in most individuals with Dup15q syndrome.
Although this website can provide general information on chromosome 15q11.2-13.1 duplication syndrome, you should always consult with your personal physician or genetic counselor for specific details on your situation.
Signs, Symptoms, and Characteristics of Dup15q syndrome
NIH 15q Duplication Syndrome Gene Review
Duplication of 15q11.2-q13.1 (Dup15q syndrome) is one of the most common copy number variations associated with autism spectrum disorders (ASD) and intellectual disability (ID).
PHYSICAL FEATURES
Since chromosomes carry genes that determine how our bodies grow and develop, having extra chromosomal material can alter a person’s physical development. Unlike many other chromosomal syndromes, there are few characteristic physical findings associated with chromosome 15q11.2-13.1 duplication syndrome.
FACIAL FEATURES
Many individuals with Dup15q syndrome share similar facial characteristics. These features are typically subtle and may be missed in infancy. These features may include:
- a flat nasal bridge with an upturned nasal tip which gives them a “button” nose
- “epicanthic” folds when the skin fold of the upper eyelid covers the inner corner of the eye
- down slanting palpebral fissures when the opening between the two eyelids slants downwards

- long philtrum: vertical groove between the base of the nose and the border of the upper lip is longer than usual
- full upper and lower lips (thick vermilion)
- palate (roof of the mouth) may be unusually high
- ears may be low-set and/or posteriorly rotated
- noticeable unfolding of the edge of the ears

- lower jaw may be smaller than normal (micrognathia)
- back of the head may be flat [Battaglia et al 1997, Borgatti et al 2001, Hogart et al 2010, Urraca et al 2013]
EARS/HEARING
Ear infections that cause fluid buildup in the middle ear are commonly reported. Hearing loss due to multiple ear infections is often temporary. However, if ear infections are left untreated during early childhood, the hearing loss can interfere with language development and worsen the speech problems associated with Dup15q syndrome.
EYES/VISION
About 30 percent of individuals with Dup15q syndrome are born with eyes that do not look in the same direction (strabismus). Strabismus can be categorized by the direction of the turned or misaligned eye: Inward turning (esotropia), Outward turning (exotropia), Upward turning (hypertropia), and Downward turning (hypotropia).
In clinical settings parents have reported diagnosis of Cortical Visual Impairment (CVI). Cortical visual impairment (CVI) is a decreased visual response due to a neurological problem affecting the visual part of the brain. A child with CVI has a normal eye exam that cannot account for the abnormal visual behavior.
GROWTH
Growth is affected in about 20–30% of individuals with Dup15q syndrome, resulting in small stature. Although puberty appears to be normal in most individuals, pubertal disorders such as central precocious puberty have been observed in some girls. (Battaglia et al [2008])
OTHER PHYSICAL CHANGES
Rarely, babies with Dup15q may be born with a cleft lip and/or palate or differences in the way their hearts, kidneys, or other body organs are formed. For this reason, it is important for newly diagnosed children with Dup15q to be carefully evaluated for the possibility of such structural differences. Hypogonadism (including undescended testicles) is reported in about 20% of affected individuals. A complete genitourinary exam is recommended for children diagnosed with Dup15q. Check with your genetics specialist for specific recommendations. (Battaglia et al [2008])
DEVELOPMENTAL
HYPOTONIA
Babies with Dup15q usually have hypotonia (poor muscle tone). They may appear “floppy” and have difficulty sucking and feeding. Motor milestones such as rolling over, sitting up, and walking are significantly delayed. Hypotonia also contributes to gross motor delays, and/or gastrointestinal issues such as constipation. Older children and adults with hypotonia often tire easily. Hypotonia in Dup15q syndrome generally decreases with age and sometimes progresses to hypertonia (tight muscle tone), particularly in the lower legs. In clinical settings, parents have reported scoliosis and hip issues.
GROSS MOTOR
Due to the hypotonia experienced by young children with Dup15q syndrome, gross motor delays are very common. Most affected children develop the ability to walk independently after age 2 or 3 (younger in children with an interstitial duplication). Individuals typically have a wide-based or uncoordinated (ataxic) pattern of walking with a slow pace and poor postural control. (Jeste etal [2020])
FINE MOTOR
Parent report suggests that fine motor delays are widespread among children with Dup15q syndrome. Nonfunctional use of objects with an immature type of exploration has been reported in the scientific literature. Delays and persistent impairment in both fine and gross motor skills affect adaptive living skills and distinguish children with Dup15q syndrome from children with a nonsyndromic autism spectrum disorder.
DEVELOPMENTAL DELAY
In early childhood most individuals with Dup15q syndrome show some degree of developmental delay/learning disabilities, ranging from mild to profound; however, it is usually in the moderate to severe range. Intellectual disability may be diagnosed after the age of 5. These cognitive disabilities are often associated with behavioral problems as children age.
SPEECH/LANGUAGE
Most children with Dup15q are affected by speech/language delays with some individuals never developing functional speech. Expressive language may be absent or may remain very poor, and is often echolalic with immediate and delayed echolalia and pronoun reversal. While the majority of children with Dup15q experience speech delays, a small subset of children are highly verbal.
In her study of Dup15q, Dr. Carolyn Schanen found 26 of 47 children had some language at the time of their participation in the research study, with the first word achieved at an average of 28.7 months (range 7-84 months) and phrase speech beginning by an average of 44.1m (range 9-114 months).
BEHAVIOR
Many children with Dup15q have difficulties with behavior and social communication, with a lack of response to social cues frequently observed. In older individuals, there is some suggestion of improving social awareness with age. Affected individuals may also experience hyperactivity, anxiety, and frustration leading to tantrums. Mood disorders and psychosis occur in some affected individuals.
AUTISM SPECTRUM DISORDERS
Although not all children with duplications develop autism the majority will likely meet clinical criteria for an Autism Spectrum Disorder (ASD). Clinical studies report that 77 – 100% of Dup15q patients are affected by autism. Manifestations of Autism Spectrum Disorder, particularly difficulties with social interaction, may increase from early to late childhood. Compared to children with nonsyndromic ASD, children with Dup15q-ASD demonstrate a distinctive behavioral profile with relative strength in items related to social interest, including preserved responsive social smile and directed facial expressions towards others – features that may inform behavioral interventions.
Chromosome 15q11-13 duplications are the most frequently identified chromosomal cause in individuals with autism (LaSalle 2023)
SENSORY PROCESSING DISORDERS
Parent reports suggest that sensory processing disorders are widespread in Dup15q syndrome. These sensory processing disorders disrupt the affected child’s ability to achieve and maintain an optimal range of arousal and to adapt to challenges in daily life. These disorders are often manifested by an over-responsiveness or under-responsiveness to sensory input or fluctuations in response to sensory input.
ATTENTION DEFICIT DISORDERS
Attention deficit disorder/hyperactivity has been reported in a number of children with Dup15q syndrome.
ANXIETY DISORDERS
Parent reports of anxiety, aggressive or self-injurious behavior in individuals with Dup15q syndrome have been noted on the Dup15q Alliance online community. More research in this area is needed.
MEDICAL
SLEEP ISSUES
Individuals with Dup15q syndrome show abnormal sleep with reduced or absent slow-wave sleep (SWS), often referred to as deep sleep, which is linked to memory. Individuals also show fewer sleep spindles or short bursts of brain activity that occur during non-REM sleep and may be involved in memory processing. Abnormal sleep may undermine cognitive development, aggravate seizures and worsen anxiety. (Saravanapandian et al [2021])
GASTROINTESTINAL ISSUES
Gastrointestinal issues throughout development are reported in Dup15q syndrome. GI symptoms were present in 76.7% of individuals with idic15 duplication and 87.5% with an interstitial duplication. Reported GI symptoms include feeding issues, gastroesophageal reflux, constipation, encopresis (stool withholding), “foamy” stools, etc. Behaviors such as irritability and aggressiveness improved with the treatment of GI symptoms in several subjects.
SEIZURE DISORDERS
Seizures represent an important medical feature of Dup15q syndrome. Over half of all people with Dup15q will have at least one seizure. Seizures most often begin between ages six months and nine years usually involving multiple seizure types including infantile spasms and myoclonic, tonic-clonic, absence, and/or focal seizures. Seizure onset can occur up through puberty and young adulthood in this population. Affected individuals may start with one seizure type, with other types emerging as the individual ages. Children with epilepsy have been found to have lower cognitive and adaptive function than those without epilepsy.
Infantile Spasms (IS): Dup15q syndrome is one of the most common known causes of infantile spasms. Infantile spasms are repetitive, but often subtle movements—such as jerking of the mid-section, dropping of the head, raising of the arms or wide-eyed blinks. Infantile spasms can be misdiagnosed as colic, reflux, or a startle reflex. As many as 40% of individuals with seizures present initially with infantile spasms; of this group, approximately 90% subsequently develop other seizure types.
Lennox Gastaut Syndrome (LGS): Infantile spasms in individuals with Dup15q syndrome often progress to Lennox Gastaut syndrome and other complex seizure patterns that may be difficult to control. LGS is characterized by recurrent seizures (epilepsy) that begin early in life. Affected individuals have multiple types of seizures, a particular pattern of brain activity (called slow spike-and-wave) measured by a test called an electroencephalogram (EEG).
Developmental Epileptic Encephalopathy (DEE): Some individuals with Dup15q syndrome may also be considered to have a Developmental Epileptic Encephalopathy. Developmental and Epileptic Encephalopathy (DEE) refers to a group of severe epilepsies that are characterized both by seizures, which are often drug-resistant, as well as encephalopathy, which is a term used to describe significant developmental delay or even loss of developmental skills.
Response to treatment is variable. Some seizures are easily controlled with the first medication, other seizures are controlled for a while and then become more complex, and some affected individuals experience intractable seizures that have never been controlled with medication. Intractable epilepsy in individuals with Dup15q may result in disabling secondary effects, including falls or developmental regression. This occurs in more than half of individuals with frequent, uncontrolled seizures or nonconvulsive status epilepticus.
INCREASED RISK FOR SUDDEN DEATH
There is an increased risk of sudden, unexpected, and currently unexplained death among children and young adults ages 7 and older with chromosome 15q11.2-13.1 duplication syndrome. The risk is a small, estimated at 0.5-1% per person per year, but significant minority. These deaths almost always occur during sleep and most (though not all) have occurred in teenagers and young adults with epilepsy. Nonambulatory status and poor seizure control appear to be risk factors for SUDEP in individuals with maternal Dup15q.
Physicians should be alert for potentially relevant symptoms and follow up with their patients according to their best clinical judgment. Benzodiazepines and barbiturates should only be used if alternatives are not available, given a possible association with sudden death in this chromosomal disorder. For more information, see the Physician Advisory Sudden Death in Chromosome 15q Duplication Syndrome.
OTHER MEDICAL PROBLEMS
Other reported medical problems include high pain threshold, recurrent respiratory infections in childhood, middle ear effusions requiring tubes, eczema, precocious puberty, other menstrual irregularities, overeating, and weight gain. Scoliosis is also reported in adolescence.

